From a research perspective, maladaptive daydreaming (MD) is still very much in it’s infancy.
As it currently stands, psychologists are still trying to determine the exact origin, triggers and causes of this condition.
Nevertheless, there are still very viable treatment options for maladaptive daydreaming, based on what we currently know about it’s symptoms and underlying driving forces.
Talking to a therapist about maladaptive daydreaming is nothing to feel ashamed of. BetterHelp has over 30,000 licensed therapists who can provide a safe space to explore your feelings, deal with compulsive thoughts and help challenge unhealthy coping mechanisms. Prices starting at $65/week. To get started with BetterHelp online therapy, click here to fill in their brief questionnaire. Discussing Psychology readers get 15% off their first month with BetterHelp.
Therapy for Maladaptive Daydreaming: What Are Your Options?
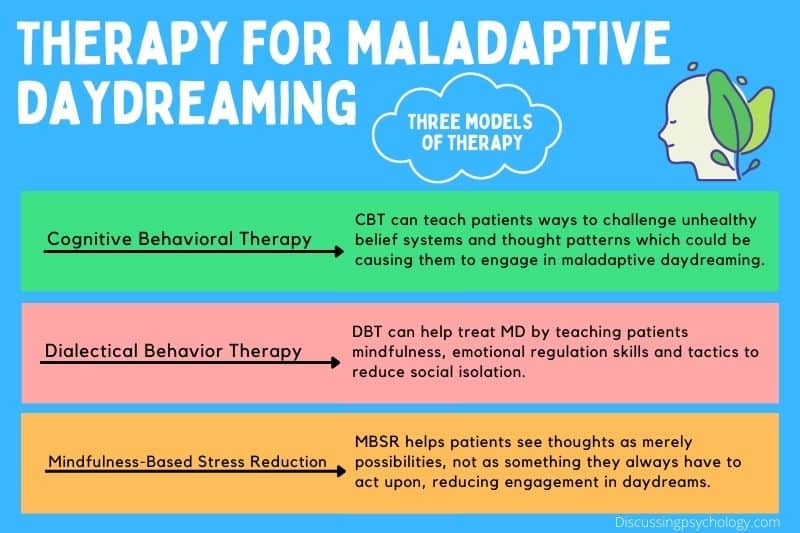
Based on our understanding of MD as a compulsive behavior used in response to stress, social isolation and a history of trauma, the most likely forms of effective treatment are those which help control compulsive thoughts and teach practical coping skills.
For this reason, possible treatment methods and therapy for maladaptive daydreaming can include:
- Cognitive Behavioral Therapy (CBT)
- Dialectical Behavior Therapy (DBT)
- Mindfulness-Based Stress Reduction (MBSR)
Cognitive Behavioral Therapy
Considered the gold standard treatment for a huge range of mental health conditions, it makes sense for CBT to be the go-to for MD as well.
CBT works on the premise that our thoughts are the link between the situations we face and our emotional and behavioral responses to them. In other words, it is how we think about challenging situations that determines how well we cope with them.
Difficult experiences can lead to our thoughts becoming distorted or unrealistic, leading us to systematically interpret situations in a way that makes them harder to deal with.
CBT teaches patients to identify when their thinking has become distorted in this way and helps them develop new, healthier ways of thinking.
CBT also places emphasis on improving behavior— teaching coping strategies to help regulate stress and improve day to day functioning, such as relaxation and interpersonal skills.
How CBT can be applied to MD:
- CBT for maladaptive daydreaming could focus on teaching alternate coping strategies so that the patient is less reliant on daydreaming as a response to difficult emotions or situations.
- Identifying unrealistic or exaggerated thought patterns caused by past traumatic experiences and adjusting them to be more adaptive. This would alleviate a patient’s distress, and therefore their need to daydream as a coping mechanism.
- Patients can learn to practice a different response when they feel an urge to daydream; for example, they may consciously choose to make their daydreams unenjoyable.
CBT is highly effective in treating a range of mental health disorders that have a high level of overlap and comorbidity with MD, such as ADHD, OCD, anxiety disorders and depression.
This makes it a likely candidate for the development of a treatment specifically tailored to tackle MD.
Dialectical Behavior Therapy
DBT was developed in the 1980s as a more specialized form of CBT used to treat borderline personality disorder (BPD). It has since been used to effectively treat other conditions including depression, PTSD, eating disorders and substance abuse.
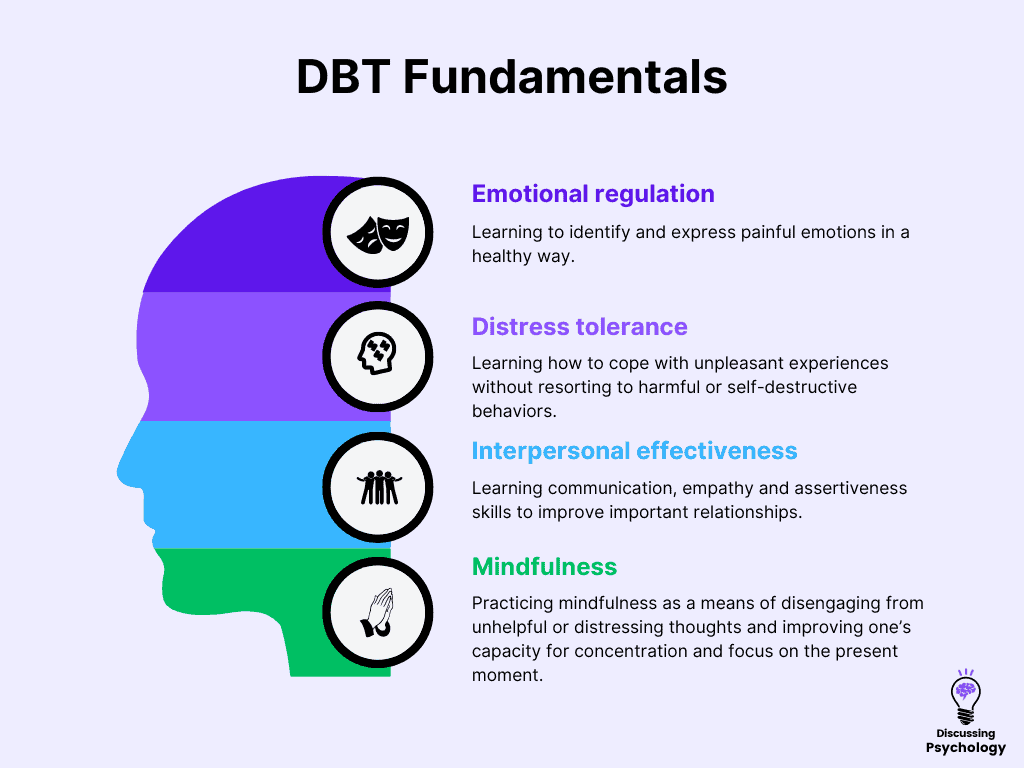
DBT shares many similarities with CBT, but focuses on the balance between learning to accept those parts of yourself and your situation you cannot control and finding ways to make positive changes where you can. The four key methods in DBT are:
- Emotional regulation: learning to identify and express painful emotions in a healthy way.
- Distress tolerance: learning how to cope with unpleasant experiences without resorting to harmful or self-destructive behaviors.
- Interpersonal effectiveness: learning communication, empathy and assertiveness skills to improve important relationships.
- Mindfulness: practicing mindfulness as a means of disengaging from unhelpful or distressing thoughts and improving one’s capacity for concentration and focus on the present moment.
Many of these principles from DBT seem ideally suited for treating MD:
- Patients can learn to regulate emotions and cope with distress without relying on daydreaming as a coping mechanism.
- Mindfulness could help patients switch off from the urge to daydream and reduce the level of uncontrollable thoughts they experience.
- Learning interpersonal skills could improve patients’ social lives, which is important since many individuals with MD report being socially isolated and using MD as a way of coping with this lack of human connection.
Since DBT has been shown to be effective in treating other compulsive behaviors and in helping people to better cope with distress, it could be a highly potent treatment for MD and is well worth further investigation.
Mindfulness-Based Stress Reduction
MBSR is a form of therapy developed in the 1970s based on the use of mindfulness meditation to reduce distress and improve one’s ability to control thought processes.
MBSR is typically delivered as an 8-week course, during which participants learn a variety of meditations and practice complementary skills such as yoga.
Mindfulness has been proven to help with a wide range of both physical and mental health conditions including:
- Anxiety
- Depression
- Addictions
- Chronic pain
- High stress levels
As noted above, mindfulness is particularly applicable to MD as it teaches patients to see thoughts as merely possibilities, not as something that they always have to act upon.
By creating a degree of mental space between a person and their thoughts, it becomes much easier to choose their own response.
For patients with MD, this means that when they feel the urge to daydream, they can choose whether to engage with this thought or not. Over time, as they choose not to engage with the urge to daydream, it becomes weaker.
It’s all about the therapist
Since it isn’t a widely recognized or understood concept, effective therapy for maladaptive daydreaming is as much about finding a therapist willing to work with your condition as it is using the right form of treatment.
Some patients with MD report that their daydreaming symptoms are dismissed or misdiagnosed by therapists who are unfamiliar with the concept, making treatment ineffective.
So if you’re looking for help getting your daydreaming under control, it’s important to find a therapist who understands what you’re going through and to give them as much information as possible to work with.
As MD continues to gain recognition and acceptance in the psychological world, the number of therapists willing to work with and treat the condition should increase.
Until then, it may be necessary to do a bit of leg work yourself to find the best fit for your treatment.
Next steps
BetterHelp has over 30,000 licensed therapists, many of whom practice therapeutic techniques such as CBT.
To get started with BetterHelp online therapy, click here to fill in their brief questionnaire.
Prices starting at $65/week. Therapy is 100% online. Cancel at anytime.
- Cherry, K. (2022, August 10). What is cognitive behavioral therapy (CBT?). Verywell Mind. https://www.verywellmind.com/what-is-cognitive-behavior-therapy-2795747#toc-effectiveness-of-cognitive-behavioral-therapy
- Harold, L. (2022, April 28). Health benefits of mindfulness-based stress reduction. Verywell Mind. https://www.verywellmind.com/benefits-of-mindfulness-based-stress-reduction-88861
- Schimelpfening, N. (2022, July 22). What is dialectical behavior therapy (DBT)?. Verywell Mind. https://www.verywellmind.com/dialectical-behavior-therapy-1067402#toc-effectiveness-of-dialectical-behavior-therapy
- Soffer-Dudek, N. (2022, May 10). Why we should take “maladaptive daydreaming” seriously. Psychology Today. https://www.psychologytoday.com/gb/blog/consciousness-and-psychopathology/202205/why-we-should-take-maladaptive-daydreaming-seriously
- Somer, E. & Herscu, O. (2017). Childhood trauma, social anxiety, absorption and fantasy dependence: Two potential mediated pathways to maladaptive daydreaming. Journal of Addictive Behaviors, Therapy and Rehabilitation, 06(04). https://doi.org/10.4172/2324-9005.1000170