Given that both maladaptive daydreaming (MD) and obsessive-compulsive disorder (OCD) stem from challenges in controlling thoughts, it’s logical to infer a potential connection between them.
Indeed, as evidence currently stands, there seems to be quite a clear symbiotic relationship between symptoms of OCD and MD. Let’s take a closer look below.
Maladaptive Daydreaming vs OCD: How Do They Differ?
Studies indicate a high comorbidity between maladaptive daydreaming and OCD, with more than half of maladaptive daydreaming patients also exhibiting symptoms of OCD.
These two conditions seem to perpetuate a cycle, where daydreaming contributes to OCD symptoms, which in turn exacerbate daydreaming tendencies.
First, let’s take a quick look at how these conditions compare. While both involve some level of intrusive or uncontrollable thoughts, the nature and experience of these thoughts is quite different.
| Obsessive-Compulsive Disorder (OCD) | Maladaptive Daydreaming (MD) |
| Difficulty controlling thoughts | Difficulty controlling thoughts |
| Thoughts pop up uncontrollably | Daydreams are consciously and deliberately entered into |
| Obsessive thoughts are short and repetitive | Daydreams can last hours and are highly elaborate |
| Thoughts are in relation to negative outcomes (contamination, illness, personal danger, etc) | Daydreams are enjoyable and content can be chosen and self-directed |
| Thoughts produce anxiety and distress | Inability to control daydreams produces anxiety and distress |
| Thoughts and compulsions make daily life much harder | Time spent in daydreaming makes daily life much harder |
While the process of obsessive thoughts leading to compulsive responses is well understood in OCD, the exact process by which MD operates is less clear.
Should daydreams be considered an obsession, given that they are recurring and hard-to-control thoughts, or are they more akin to compulsions, in that the afflicted person feels a strong urge to engage with them?
What’s the Link Between Maladaptive Daydreaming and OCD?
MD is known to have high rates of comorbidity with various other mental health conditions, such as ADHD, anxiety, and depression.
OCD is near the top of the list, with just over half (53%) of patients with MD also experiencing some form of obsessive-compulsive condition.
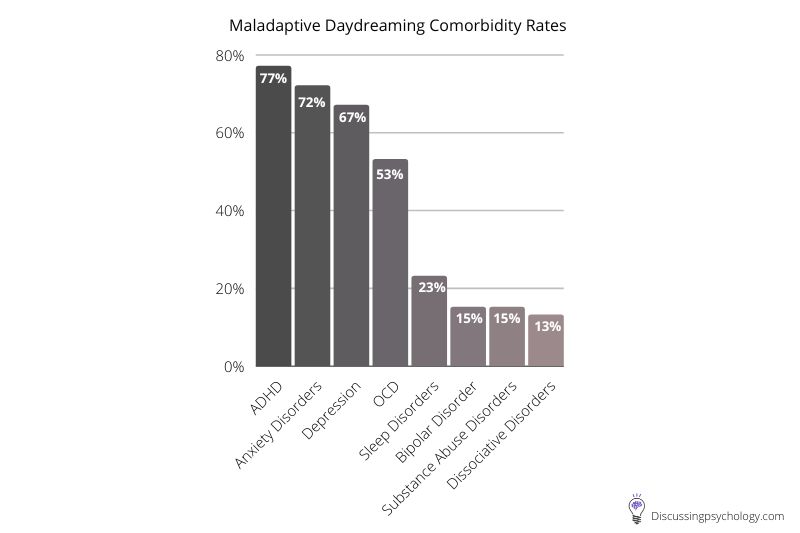
These levels of overlap suggest some connection between the two conditions, either in terms of risk factors or the underlying mechanisms leading to symptoms.
But what exactly is the relationship? Does one condition cause the other, or are they perhaps both caused by shared experiences and personality traits?
A Deeper Look into the Relationship
To get a better understanding of the link between maladaptive daydreaming and OCD symptoms, MD researchers Eli Somer and Nirit Soffer-Dudek recruited 77 individuals with MD and asked them to keep a daily diary for two weeks.
This diary recorded the time they spent daydreaming, their levels of various mental health symptoms, and their mood at different times of day.
It was found that when participants engaged in daydreaming, they experienced significantly lower mood and significantly higher obsessive-compulsive symptoms the following day.
Obsessive-compulsive disorder symptoms were also found to precede periods of daydreaming. In other words, OCD-like symptoms appear to be both a cause and consequence of prolonged daydreaming.
A cycle of symptoms
Previous research has identified a link between absorptive dissociation — getting so caught up in your own thoughts that you lose track of the real world — and symptoms of OCD.
This is thought to be because when one comes out of a period of absorption it may be unclear what’s happening or how much time has elapsed, leading to the need to mentally check where you are, what you’re supposed to be doing, and so on.
It is also known that repeated checking and ritualized thoughts or actions, such as those present in obsessive-compulsive disorder, produce a sense of derealization and depersonalization: You experience a lapse in the sense of who you are and what is real.
Both absorptive dissociation and OCD symptoms are also commonly reported to produce negative emotions such as worry, guilt, shame, or frustration.
Taking all of this together, a cycle emerges in which daydreaming leads to symptoms of OCD, which leads to derealization, making further daydreaming more likely.
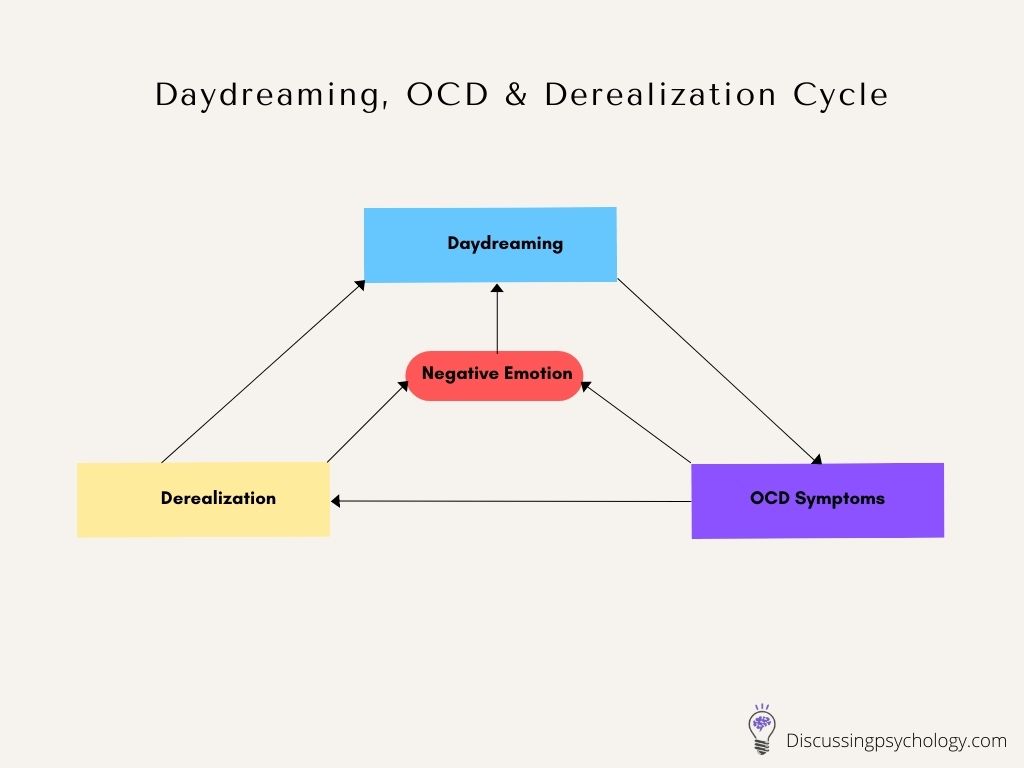
Both derealization and OCD symptoms can also lead to negative emotions, which can make a person more likely to engage in daydreaming as a means of coping or distraction.
This cycle suggests that maladaptive daydreaming and OCD feed off each other repeatedly, while also producing a constant stream of worry, low mood, and shame.
Which comes first?
This cycle provides a plausible explanation of how maladaptive daydreaming and obsessive-compulsive disorder interact once both are present.
However, an important and currently unanswered question is which causes which.
Research into this is still ongoing, but the model above suggests several potential in-roads that could kick start the cycle of symptoms:
- Daydreaming could be used as a coping mechanism or distraction to deal with obsessive thoughts and the distress they cause, eventually becoming a compulsion itself.
- OCD could lead to increased sense of derealization over time, leading to increased time spent daydreaming.
- Daydreaming and absorption may cause a person to frequently need to engage in mental checking, which over time, could become a compulsive habit.
Hope for the future
The discovery of this link between OCD and symptoms of maladaptive daydreaming also offers a glimmer of hope for people living with MD in that it suggests a possible treatment.
As with all vicious cycles, the trick is finding ways to break one of the links and thereby stop the cycle.
Reducing OCD symptoms
For patients with OCD this is done through a process called exposure and response prevention: The patient experiences the conditions in which their obsessive thoughts appear but tries not to respond with their compulsive thoughts or actions.
Often this is done by intentionally refocusing yourself on a different response rather than simply trying to block out the compulsion.
Reducing MD symptoms
A similar approach could be taken with maladaptive daydreaming. When a patient with MD feels the urge to daydream, they could instead respond with a different thought or action.
One case study reported some success with a rather drastic application of this technique: Whenever the patient felt himself slipping into a daydream, he would intentionally change the dream to be less enjoyable by imagining characters dying or other negative endings to the narrative.
While convincing people with MD to kill off their beloved fantasy characters may be a hard sell, if techniques such as these can disrupt the cycle of dreaming, OCD symptoms and negative emotions, it may be a trade worth making.
- Fergusson, S. (2019, October 28). Can excessive daydreaming be a symptom of mental Illness? Healthline. https://www.healthline.com/health/mental-health/excessive-daydreaming-symptom-of-mental-illness
- Fields, L. (2020, September 4). Obsessive-compulsive disorder (OCD). WebMD. https://www.webmd.com/mental-health/obsessive-compulsive-disorder
- Soffer-Dudek, N., & Somer, E. (2018). Trapped in a daydream: Daily elevations in maladaptive daydreaming are associated with daily psychopathological symptoms. Frontiers In Psychiatry, 9. https://doi.org/10.3389/fpsyt.2018.00194
- Somer, E. (2018). Maladaptive daydreaming: Ontological analysis, treatment rationale; a pilot case report. Frontiers in the Psychotherapy of Trauma and Dissociation, 1, 1-22. https://doi.org/10.XXXX/ftpd.2017.0006