A key challenge that comes with treating maladaptive daydreaming is that it frequently co-exists with other mental health disorders.
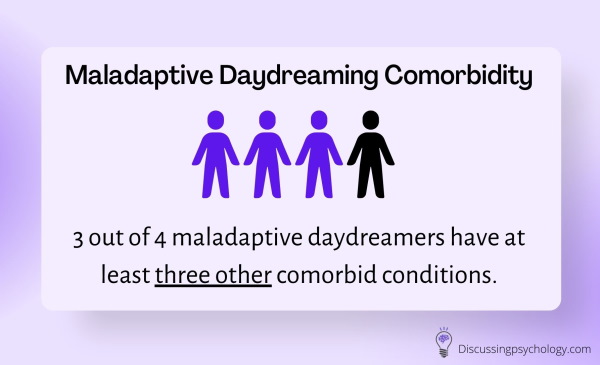
It’s estimated a whopping 3 out of every 4 maladaptive daydreamers have at least three other comorbid conditions. This is quite an alarming statistic—and one that continually proves to be a significant hurdle for therapists and daydreamers alike.
But what exactly are the most common conditions diagnosed alongside maladaptive daydreaming? Let’s take a closer look at the comorbidity rates below.
Maladaptive Daydreaming Comorbidity Rates
Maladaptive daydreaming (MD) has high levels of comorbidity with other mental health disorders including:
- ADHD (77%)
- Anxiety disorders (72%)
- Depression (67%)
- OCD (53%)
- Sleep disorders (23%)
- Bipolar disorder (15%)
- Substance abuse disorders (15%)
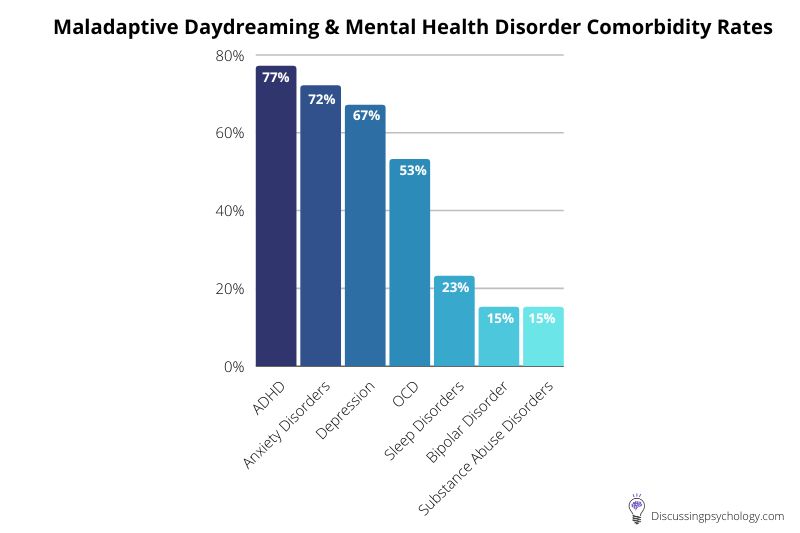
A study in 2017 by Eli Somer (the original psychologist to coin the term Maladaptive Daydreaming) and colleagues assessed 39 people who experienced high levels of intrusive fantasies for the presence of other mental health disorders.
Very high rates of comorbidity with maladaptive daydreaming were found in almost all the study participants.
Roughly three quarters (74.4%) were living with three additional mental health conditions, while just over 40% met the criteria for four.
Let’s look at the rates for the most commonly comorbid disorders.
Maladaptive Daydreaming & ADHD
In the aforementioned study, 76.9% of the participants were also living with Attention-Deficit Hyperactivity Disorder (ADHD), making it the most common comorbid condition with MD.
27 of the 30 patients with ADHD were diagnosed with the inattentive subtype, a form of the condition in which the main symptoms are difficulties maintaining your attention, getting easily distracted, and organization difficulties.
High levels of daydreaming are a common characteristic — though not a diagnostic requirement — for inattentive ADHD.
This link between inattentive ADHD and maladaptive daydreaming makes a lot of sense because both conditions involve a recurring inability to focus on real world tasks due to a compulsive need to attend to mental distractions.
In both conditions, this tendency towards distraction causes significant impairment and can make work, education, and daily tasks difficult.
Are ADHD & Maladaptive Daydreaming Linked?
Given the extremely high rates of comorbidity between ADHD and MD it’s tempting to think of them as being linked on a deeper level, perhaps even different manifestations of the same underlying condition.
There are, however, important differences:
- MD often involves a kinesthetic component which is absent in ADHD; patients will physically act or position themselves in certain ways to better facilitate their daydreams, and they often use music to trigger deeper involvement in their fantasies.
- The daydreaming typical of people with ADHD is often described as ‘mind wandering’—thoughts repeatedly jumping from one thing to the next—whereas with MD they are systematically engaging with an elaborately developed fantasy world.
This has led researchers to hypothesize that MD may contribute to the development and symptoms of ADHD, but the reverse is not true: ADHD cannot be a contributing factor to MD.
Maladaptive Daydreaming & Anxiety Disorders
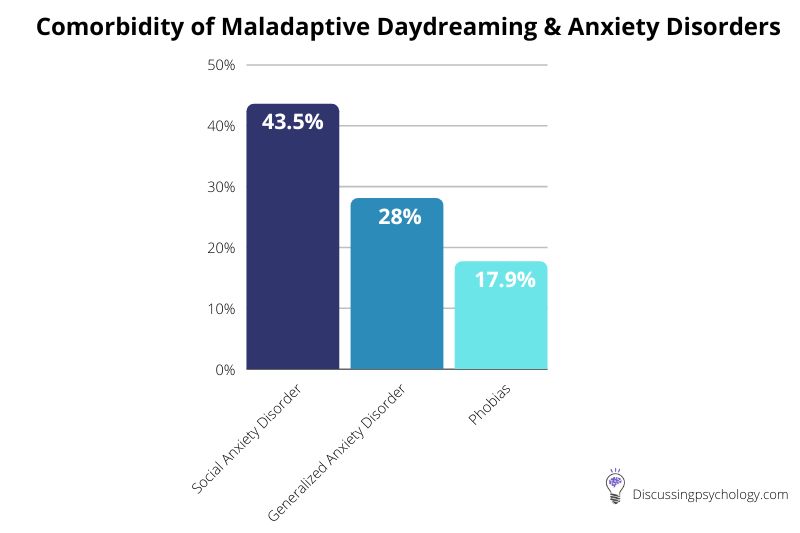
In Somer’s 2017 comorbidity study, 71.8% of participants met the criteria for one or more anxiety disorders, as shown in the below pie graph.
Further study is needed to understand the exact nature of this comorbidity relationship.
It is known that MD is often driven by a feeling that the need for intimacy, recognition and belonging are not being met in real life and so turning to fantasies is a form of fulfillment.
It is therefore possible that social anxiety could lead to isolation and loneliness, leading to increased use of daydreaming.
Alternatively, MD could lead to impaired social relationships, leading to greater anxiety in social situations.
In this sense, it could be said that social anxiety and maladaptive daydreaming are two conditions which may feed off one-another when left untreated.
Likewise, high comorbidity with Generalized Anxiety Disorder (GAD) and other anxiety disorders may reflect the distress caused by MD, or MD may be a coping mechanism used to alleviate the distress of these conditions.
Maladaptive Daydreaming & Obsessive-Compulsive Disorder (OCD)
A little over half (53%) of participants were diagnosed with OCD, a condition characterized by recurrent distressing thoughts (obsessions) and actions designed to resolve or ‘fix’ these unwanted thoughts (compulsions).
Often these compulsions are purely cognitive, for example, imagining yourself in a certain way or going through a mental list of safety checks in order to reduce anxiety.
Recurring, uncontrollable thoughts are a common feature of both maladaptive daydreaming and OCD.
However, the compulsive fantasies triggered by MD are not an attempt to reduce the anxiety caused by other obsessive thoughts. This suggests that although they share some common features, MD and OCD are distinct conditions.
A recent study conducted in 2022 found that maladaptive daydreaming may have a prevalence rate of 2.5%. This means it could be more than twice as common as OCD in the general population, with OCD affecting only 1.2% of the population over any given 12-month period.
Maladaptive Daydreaming and Psychosis
Interestingly, recorded levels of psychosis among the participants was low.
This suggests that while MD involves a high level of engagement with stories and characters outside of the real world, the line between what is real and what is imagined is rarely blurred.
Imagined Lives, Real Distress
The fact that MD has such high rates of comorbidity with, but is distinct from, other mental health disorders leads Somer and his colleagues to conclude that it is a separate mental health condition, the significance of which is often overlooked by therapists.
Regardless of the debate around diagnosis, classification, and comorbidity, the bottom line is that maladaptive daydreaming causes significant suffering for those afflicted with it.
40% of study participants with MD were unable to hold down a job due to their condition, while 28% had attempted suicide.
Treating related disorders may help reduce the symptoms of MD, but treatment by proxy is unlikely to ever be fully effective.
Developing our understanding of what causes, drives and maintains maladaptive daydreaming to the point where effective treatments can be developed is therefore a high priority for future study.
- Ellwood, B. (2022, April 27). Study suggests maladaptive daydreaming should be classified as a unique mental disorder, distinct from ADHD. PsyPost. https://www.psypost.org/2022/04/study-suggests-maladaptive-daydreaming-should-be-classified-as-a-unique-mental-disorder-distinct-from-adhd-63025
- Schimmenti, A., Somer, E., & Regis, M. (2019). Maladaptive daydreaming: Towards a nosological definition. Annales Médico-Psychologiques, Revue Psychiatrique, 177(9), 865–874. https://doi.org/10.1016/j.amp.2019.08.014
- Somer, E., Soffer-Dudek, N., & Ross, C. (2017). The comorbidity of daydreaming disorder (Maladaptive Daydreaming). Journal Of Nervous &Amp; Mental Disease, 205(7), 525–530. https://doi.org/10.1097/nmd.0000000000000685
- Somer, E., Somer, L., & Jopp, D. (2016). Parallel lives: A phenomenological study of the lived experience of maladaptive daydreaming. Journal of Trauma and Dissociation, 17(5), 561–576. https://doi.org/10.1080/15299732.2016.1160463
- Watson, S (2020, July 13). ADHD: Inattentive Type. WebMD. https://www.webmd.com/add-adhd/childhood-adhd/adhd-inattentive-type