Both maladaptive daydreaming (MD) and schizophrenia are marked by a severe disconnection from physical reality.
This has led to speculation that the two disorders may be linked in some way. Or, at the very least, one may lead into the development of the other.
But does this logic hold up in the world of psychology? Is there any research supporting this idea?
Maladaptive Daydreaming and Schizophrenia: Is There a Connection?
Research has yet to find any link between either condition, with there being no evidence that maladaptive daydreaming can lead to schizophrenia. The key difference is that people with MD know they are dreaming, while patients with schizophrenia perceive their hallucinations as real.
Let’s start with the numbers. A 2017 study assessed 39 individuals with MD for the presence of a wide range of other mental health conditions.
High rates of comorbidity were found—in fact, just under 75% of the study participants met the criteria for at least three additional disorders.
The most commonly comorbid disorders were:
- ADHD (77% of participants)
- Anxiety disorders (72%)
- Depressive disorders (67%)
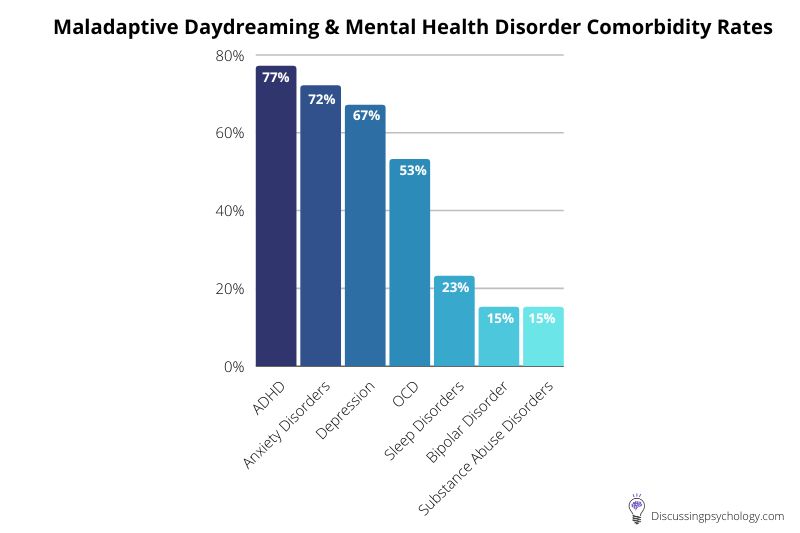
In comparison, just one participant in the study met the criteria for a diagnosis of schizophrenia.
So while MD is indeed linked to a variety of other mental health conditions, worries that it could also lead to schizophrenia appear unfounded.
Of course, one study with a relatively small number of subjects is hardly sufficient evidence to totally rule out a link.
But based on these initial findings, it is possible to speculate on why these two conditions appear separate.
Though they share some surface level similarities in symptoms, the experiences of individuals with MD and those with schizophrenia are actually very different.
Daydreams vs Hallucinations: How Do They Differ?
To illustrate this, let’s look in more depth at the daydreams typical of a patient with maladaptive daydreaming compared to the hallucinations found in those with schizophrenia.
Though both involve a level of dissociation or detachment from real sensory experience, the similarity ends there.
| Point of Difference | Maladaptive Daydreaming | Schizophrenia |
| Reality Testing | Daydreams are not confused with reality — patients know their daydreams are not real. | Difficulty separating fantasy from reality due to vivid hallucinations and delusions. |
| Degree of Control | Daydreams are controllable, starting with a conscious choice. | Hallucinations and delusions are out of a patient’s control. |
| Experience | Daydreaming can be an enjoyable experience. | Symptoms of schizophrenia are often distressing and very rarely described as enjoyable. |
Let’s take a look at each point of difference between maladaptive daydreaming and schizophrenia in more detail below.
Daydreamers Know That Their Dreams Aren’t Real
One of the core symptoms of schizophrenia is a difficulty in separating fantasy from reality.
Patients often experience vivid hallucinations and delusions as though they were real parts of their sensory experience.
This is caused by impairments to reality monitoring— a system in the brain responsible for checking whether your experiences were generated internally by your imagination or externally in the real world.
Daydreams, by contrast, are never experienced as being real, even amongst people whose daydreaming takes on a compulsive and disruptive nature. Patients with MD may struggle to control their desire to daydream, but they are never in any doubt as to whether their fantasies are real or not.
This is arguably the core difference between MD and psychotic disorders such as schizophrenia: Maladaptive daydreamers know they are dreaming, while schizophrenics do not.
Daydreams Are Controllable
While the urge to daydream may be a constant battle for people with MD, the actual act of dreaming is under their direct control.
That is, people with MD can consciously choose when to start daydreaming, often using triggers such as music or repetitive motion to facilitate their fantasies.
Once absorbed in their daydreams, MD patients can normally choose what happens in their fantasies.
This is a big part of the appeal of spending hours at a time in these daydreams: getting to live out stories and experiences that grant the dreamer a sense of power, recognition, or satisfaction that they otherwise find lacking in their lives.
This ability to control the initiation and content of daydreams is in stark contrast to the hallucinations experienced by patients with schizophrenia.
Hallucinations typically bleed into reality seamlessly, to the point where distinguishing real stimuli from those created by one’s mind becomes challenging.
Since they perceive them as simply a part of reality, patients with schizophrenia also have no direct control over the content of their hallucinations.
Daydreams Are Enjoyable
Finally, people with MD choose to engage with their daydreams because they are an enjoyable, pleasant experience.
Becoming absorbed in fantastical stories where you are the central character and control every aspect of the world is an enjoyable experience for many, particularly if their real lives have been traumatic or unsatisfying.
As one MD patient described it:
“Imagine a television show that kept getting renewed year after year for 30 years. Think of all the experiences you would have watched the characters go through. That is what my mind has been doing for over 30 years.”
The content of hallucinations in schizophrenic patients varies greatly between individuals, but few would describe the experience as enjoyable.
People with schizophrenia may experience:
- Sudden voices telling them to do things.
- Distorted images of people or objects.
- Other sensory stimuli only they can perceive.
Often these hallucinations are highly distressing in nature, revolving around delusions of being persecuted by unseen forces or thinking that others are in control of one’s life.
Even when this is not the case, the sudden and intrusive nature of these hallucinations, and the very fact that the person is experiencing something which only they can perceive makes hallucinations inherently frightening to go through.
Additional Symptoms of Schizophrenia
When comparing maladaptive daydreaming to schizophrenia, it’s also worth pointing out that hallucinations are just one of the common symptoms of the latter condition.
Other symptoms of schizophrenia which bear no relation to maladaptive daydreaming include:
- Disorganized thinking: the inability to control thoughts, impaired concentration, memory issues and difficulty following conversations.
- Speech impairment: this inability to focus and think clearly can lead to impairments in communicating, such as zoning out or jumbled speech.
- Flattening: difficulty experiencing and conveying emotion and a lack of pleasure and enjoyment in life.
- Struggles with daily functioning: the impairments to thinking and memory can be so severe that a person’s ability to perform simple daily tasks is limited.
Dreams or Nightmares
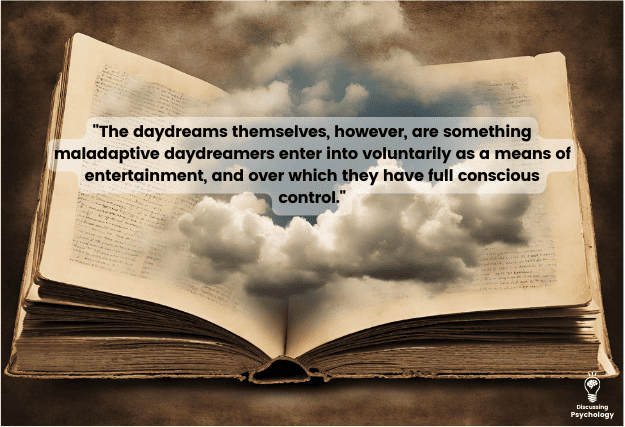
Maladaptive daydreaming is a condition that causes severe distress, has strong links to other mental illness, and even increases a patient’s risk of suicide.
The daydreams themselves, however, are something patients enter into voluntarily as a means of entertainment, and over which they have full conscious control.
They also know that they are daydreaming, however much they may prefer their daydreams to their reality.
The hallucinations caused by schizophrenia are far more akin to nightmares: They are sudden, uncontrollable and terrifying.
While people with MD use their daydreams as an escape from reality, no such respite is possible for people with schizophrenia for whom reality has become so warped and distorted that living a normal life becomes almost impossible.
- Bigelsen, J., Lehrfeld, J., Jopp, D. and Somer, E., 2016. Maladaptive daydreaming: Evidence for an under-researched mental health disorder. Consciousness and Cognition, 42, pp.254–266. https://www.sciencedirect.com/science/article/abs/pii/S1053810016300460
- Bigelsen, J., & Schupak, C. (2011). Compulsive fantasy: Proposed evidence of an under-reported syndrome through a systematic study of 90 self-identified non-normative fantasizers. Consciousness And Cognition, 20(4), 1634–1648. https://doi.org/10.1016/j.concog.2011.08.013
- Cuncic, A. (2022, February 26). What are paranoid delusions? Verywell Mind. https://www.verywellmind.com/what-are-paranoid-delusions-5218314
- D’Arrigo, T (2020, December 13). What are the symptoms of schizophrenia? WebMD. https://www.webmd.com/schizophrenia/schizophrenia-symptoms
- Garrison, J., Fernandez-Egea, E., Zaman, R., Agius, M., & Simons, J. (2017). Reality monitoring impairment in schizophrenia reflects specific prefrontal cortex dysfunction. Neuroimage: Clinical, 14, 260–268. https://doi.org/10.1016/j.nicl.2017.01.028
- Somer, E., Soffer-Dudek, N., & Ross, C. (2017). The comorbidity of daydreaming disorder (maladaptive daydreaming). Journal Of Nervous and Mental Disease, 205(7), 525–530. https://doi.org/10.1097/nmd.0000000000000685